This weekend I had the pleasure of attending the Science of Ball Rolling (funny name, great course) led by Jill Miller, the creator of Yoga Tune-Up and the Roll Model Method, and author of the book, The Roll Model: A Step-By-Step Guide to Erase Pain, Improve Mobility, and Live Better in Your Body
The weekend proved to be one of the most rewarding and relaxing of my life. Set in the beautiful, serene environment of the Kripalu Center in Stockbridge, Massachusetts, the weekend was formatted as more of a yoga retreat than a continuing education class. By course's end, I found myself calmer, more knowledgable, and both grateful to the individuals pioneering change in the movement professions and hopeful for the future of health and wellness in our society.
Before attending the course, I was a little skeptical that I would learn much from the experience, as I have read Jill's book and have already been utilizing her techniques for over a year to much success with patients and clients. However, something told me that being in the presence of the creator of such great work would offer knowledge and inspiration that I could not predict. I was not disappointed! Jill and her colleagues, expertly described- through lecture and movement practices - how a simple grippy, pliable rubber ball can change the momentum of your entire day in an instant.
The key to the educational process of the weekend, was gaining a practical and functional understanding of the role of fascia in self soft tissue work. Jill described three major factors of improved well being when one takes good care of his/her fascia.
1. MOBILITY
In a very clever and effective manner (that spoke to my kinesthetic manner of learning), Jill utilized four class participants and resistance bands in order to display the interwoven relationship of the fascia to muscle (see Treat While You Train: Self-Care Kit Instructional DVDs with Jill and Dr. Kelly Starrett for demonstration).
She also made the class repeat the important concept that one "can have fascia without muscle, but cannot have muscle without fascia". This concept brings to light the fact that any change made to muscle must include a change to the fascia.
During the course, changes in mobility were discussed from a theoretical basis, with a video demonstration where Dr. Gil Hedley (http://www.gilhedley.com/ghabout.php) navigated a human cadaver and explained the importance of regular movement of the body's tissues in order to restore sliding surfaces between muscles by routinely breaking up the fascial "fuzz".
This "fuzz" becomes much more difficult to break down with frequent inactivity of specific body regions, which leads to chronic immobility and pain. Generally speaking, the balls are meant to get into those “sliding surfaces” and break down the "fuzz" in a very localized manner in order to restore normal tissue mobility.
Anytime, theoretical mechanisms of change to human anatomy and physiology are described, there is always an opportunity for eye rolling and second guessing. In my experience as a physiotherapist and strength and conditioning professional, I have yet to meet two professionals with the exact same theoretical basis for the interventions they perform. Regardless, of where one stands in terms of theoretical understanding, it is hard to argue with obvious physical change in your own body. This was demonstrated in abundance throughout the weekend. Every technique and sequence that was performed was preceded by a “check-in” to assess one’s body pre-intervention, and then followed by a “check-out” to observe the after effects of the self care work. In my own practice, there was not one sequence that did not make substantial change from before to after, and looking around the room it was obvious to see that I was not the only participant with this experience. The most surprising change I experienced was dropping into a “thigh-to-calf” squat with my feet facing forward after about 5 minutes of rolling out my feet. Typically, the chronic tightness in my ankles make it impossible to keep my heels down in that position, but that did not seem to be an issue after the footwork.
2. PROPIOCEPTION
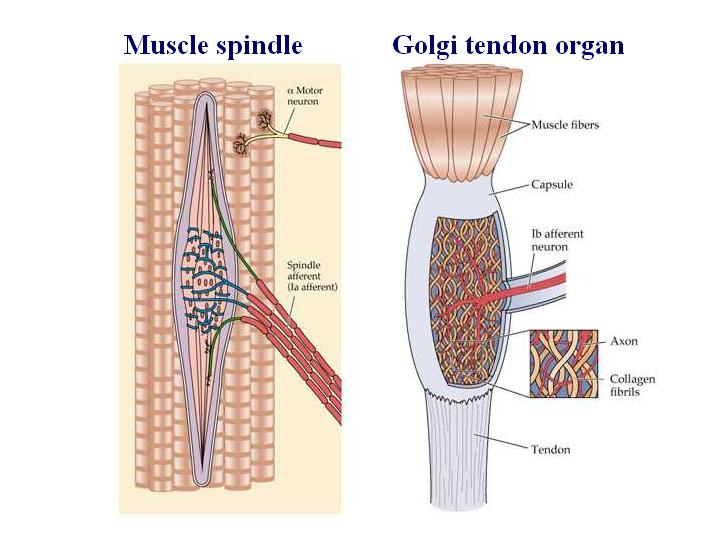
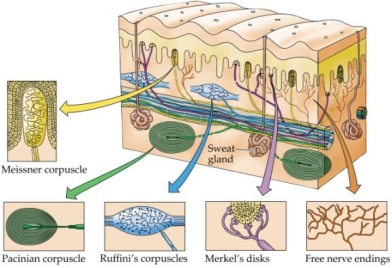
Jill defined proprioception as the body’s inner sense of itself (or inner GPS). She went on to describe in detail the rich supply of proprioceptors comprised within fascial tissue. She noted that fascial tissue contains up to 6x more proprioceptors than any other tissue in the body. Jill defined five different mechanical proprioceptors (mechanoreceptors) in the body: 1. Muscle spindles; 2. Golgi tendon organs (GTOs); 3. Pacinian corpuscles; 4. Ruffini endings; and 5. Interstitial fibers. Stimulation of all of these receptors lead to a better understanding of where the body is in space. Practically this means that one gains a better appreciation of their own anatomy and posture. This leads to an improved ability to activate dormant muscles and inhibit the use of overactive ones that experience chronic tension. Moreover, improved proprioception allows for improved quality of movement, therefore decreasing risk for and/or enhancing recovering from injury.
3. RELAXATION
Diving deeper into the functions of the mechanoreceptors, Jill explained that along with creating improved awareness of one’s body, these receptors also create either local or systemic relaxation. The muscle spindles and GTOs respond to tissue stretch and resistance to create relaxation and lengthening in the muscle belly and tendons. Pacinian corpuscles respond to oscillatory/vibratory pressures to create local tissue relaxation, while Ruffini endings respond to deep, sustained, oblique pressures to create more systemic (central/autonomic nervous systems) changes. Interstitial fibers, when stimulated with either rapidly changing pressure or sustained pressure, create changes in circulation (increase in blood flow) and pain (good and bad). Moreover, in addition to promotion of local tissue and nervous system relaxation, stimulation of these proprioceptors through use of the balls creates a decrease in pain receptor (nociceptor) activity. This is due to the much quicker speed in which the proprioceptors are stimulated relative to the pain receptors. Therefore, utilizing the balls to promote increased proprioceptive activity can create substantial reductions in pain.
Further enhancing the weekend experience, Jill and her whole staff impressed me with their accessibility. Jill seemed to go out of her way to personally get to know the course participants, which is impressive for a mobility rockstar or "roll-star" like herself.
In conclusion, self myofascial work has proven to be one of the most effective treatment tools in both my personal movement practice and that of my patients and clients. Jill Miller's work blends a high level of education, with easy-to-utilize practicality. Check out Jill and her programs at: https://www.yogatuneup.com.